PCOS 101: What Every Woman Should Know About Hormones and Insulin
I'm coming in hot today. 🔥
We need to talk about PCOS.
Why? Because research shows 50–70% of women with PCOS are undiagnosed. And if that stat feels unbelievable—well, I personally became part of it last summer.
I knew the symptoms. I’d had many of them in high school before they were hidden under the hormonal birth control I started at 15. Years ago, I changed my lifestyle to support my blood sugar, and those symptoms vanished—so I never really labeled myself as having PCOS.
Then… a stressful season hit. And suddenly:
Acne
Weight gain
Waking up at 2 a.m.
Irregular cycles
So, I did what any logical person would do—marched into my OBGYN’s office and told her I had PCOS. She didn’t believe me at first—said I was “too lean”—but since we go way back from my Labor & Delivery nurse days, she humored me and ordered an ultrasound.
A week later, I’m sitting across from her, and she’s saying, “You were right. Your ultrasound is textbook PCOS.”
I share this because I want you to know: You are the expert on your body. Your doctor might see you for 30 minutes a year. You’re with yourself every second of every day. Listen to what your body is telling you.
Here’s what’s wild:
1 in 5 women may have PCOS.
Causes? Could be genetics—but often linked to insulin resistance and stress.
PCOS is a leading cause of infertility.
It’s not just about ovaries—it’s about metabolism, hormones, and your whole body.
Here's the breakdown on PCOS and Insulin Resistance:
Prevalence — Around 70–80% of women with PCOS have some degree of insulin resistance, even if they aren’t overweight.
Mechanism — When cells don’t respond well to insulin, the body pumps out more insulin to keep blood sugar stable.
Hormonal Cascade — High insulin levels stimulate the ovaries to produce more androgens (like testosterone), which disrupts normal ovulation and can lead to irregular cycles, acne, and excess hair growth.
Vicious Cycle — Elevated androgens and disrupted ovulation make it harder to regulate insulin, so the cycle feeds itself unless addressed.
Why it matters for PCOS treatment — Improving insulin sensitivity (through diet, movement, stress regulation, and sometimes medication) can help restore ovulation, reduce symptoms, and improve fertility.
BUT HERE'S THE GOOD NEWS—it’s often reversible.
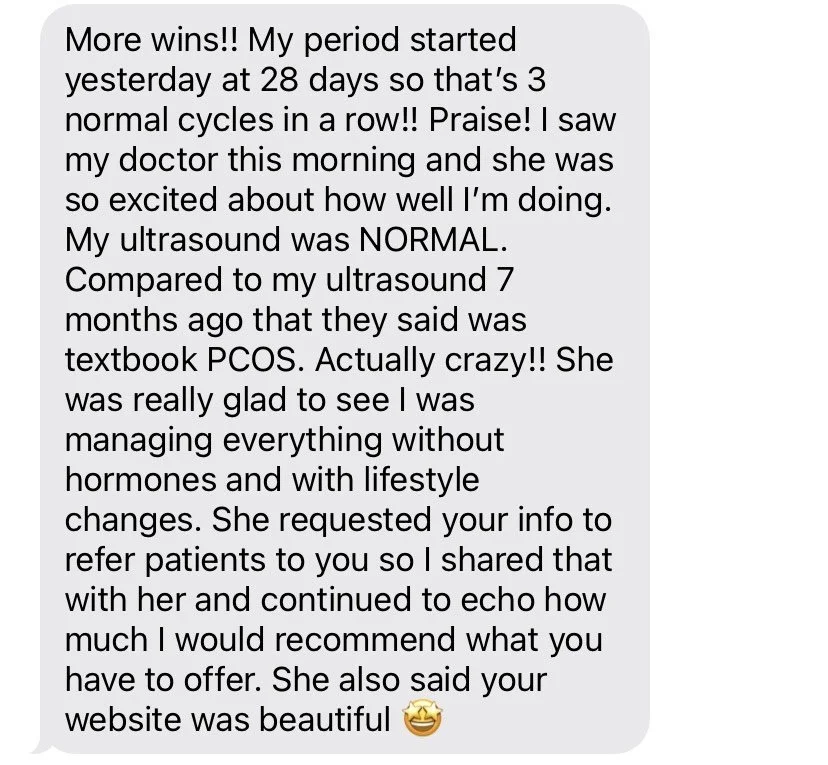
One of my clients just had a follow-up ultrasound after 3 months of working together—all of her cysts were gone. (which btw she did this in the busyness of summer and traveling and fun…just saying.)
All of this to say, your health is in your hands. No one can do it for you.
Start tuning in.
Start learning your body’s signals.
Start now.
If you are ready to know your body better than anyone else and feel good in your body again, click here to apply to work with me. There’s never a perfect time, but now is as close as it can get.